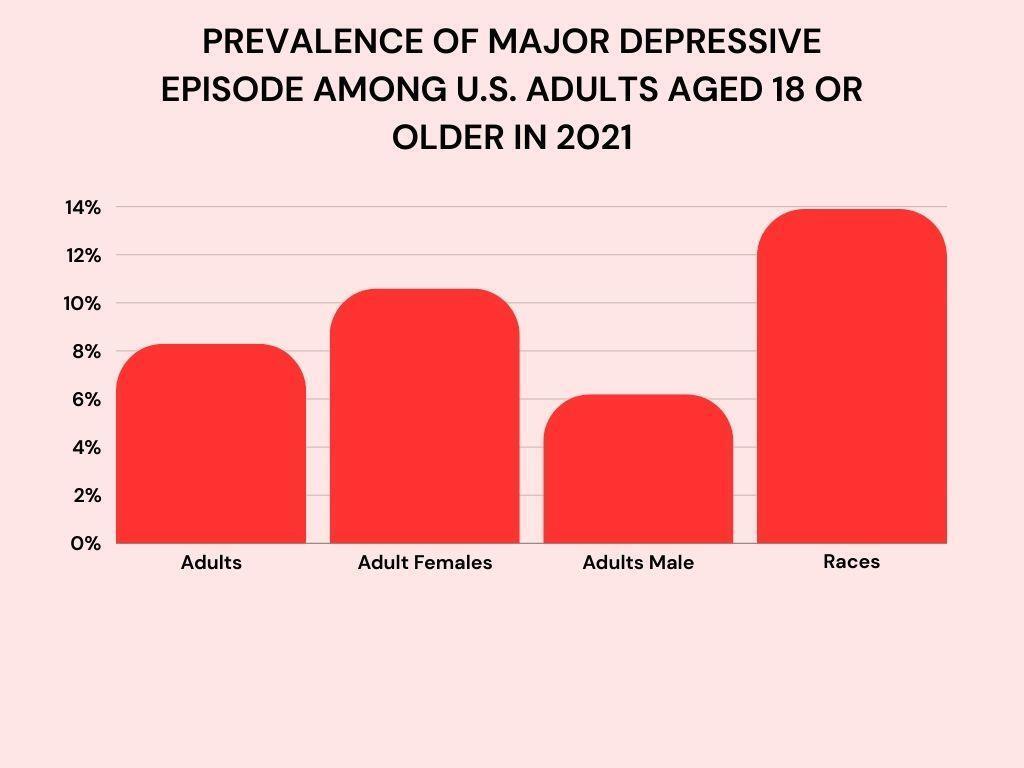
Drug use and mental health have a complex, bidirectional relationship. Recent studies indicate that nearly 50% of individuals with a substance use disorder also experience mental illness. It is critical to understand how different drugs impact mental health both in the short and long term.
This article delves into the interaction between commonly abused substances and mental wellbeing, covering treatment approaches, prevention strategies, recovery stories, and future research directions.
The Interplay Between Drugs and Mental Health
Drug use can significantly impact mental health in several ways, with effects ranging from short-term alterations in mood and cognition to long-term psychiatric disorders. Conversely, the use of drugs can exacerbate underlying mental health conditions, creating a vicious cycle that can be challenging to break. Understanding this complex interplay is crucial for effective treatment and prevention strategies.
The connection between drug use and mental health is intricate and often leads to some of the worst drug addiction scenarios. Mental illnesses like depression and anxiety frequently precede addiction, making individuals more susceptible to abusing substances as a form of self-medication.
This pattern of use can quickly escalate to severe addiction, often considered among the worst due to its profound impact on mental health.
For example, heavy marijuana use is associated with an increased risk of developing psychosis and schizophrenia in those with a predisposition to mental illness. On the other hand, controlled medicinal marijuana use can alleviate certain psychiatric symptoms like anxiety. The effects vary based on dosage, duration of use, genetics, and more.
Grasping these nuanced relationships for various substances is crucial for understanding their short- and long-term effects on mental health.
Psychopharmacology of Commonly Misused Substances
The specific psychopharmacological effects of different drug classes like stimulants, opioids, and depressants influence their impact on mental health.
Stimulants
Stimulants like cocaine and methamphetamines increase dopamine levels, enhancing alertness and attention initially. However, chronic, high-dose use can trigger psychosis, aggression, and impulsivity.
Opioids
Opioids provide pain relief and euphoria by activating the brain's natural opioid receptors. Short-term use has limited effects, while prolonged use can decrease dopamine activity, contributing to depression and apathy.
Depressants
Alcohol, benzodiazepines, and other depressants slow down the central nervous system. Excessive use often leads to poor concentration, irritability, loss of inhibition, and memory problems over time.
Understanding the distinct mechanisms of each substance offers insight into their mental health risks and ways to mitigate them.
Long-Term Impacts of Drug Use on Mental Health
Chronic substance abuse can have lasting consequences by altering brain structure and function. These brain changes may persist even after quitting the drug. For example, studies show that long-term methamphetamine use damages dopamine and serotonin neurons, which can impair verbal learning, memory, and emotional processing.
Chronic alcoholism is linked to structural damage and neuroinflammation. This can impair judgment, cognition, mood regulation, and impulse control, leading to mental disorders like depression.
While not all drug-induced brain changes are irreversible due to the brain's plasticity, significant psychiatric effects can persist long after quitting. Managing these requires a combination of therapy and medications.
Treatment Approaches: Balancing Medication and Therapy
Integrated treatment plans that blend psychotherapy with prescription medications as needed deliver the best outcomes for co-occurring mental health and substance use disorders (9).
Cognitive behavioral therapy helps modify thoughts and behaviors that trigger drug use by teaching coping skills. Support groups provide social reinforcement for abstinence. Meanwhile, medications like antidepressants and mood stabilizers can alleviate underlying psychiatric symptoms.
A tailored treatment plan combining psychosocial and pharmacological interventions customized to an individual's needs is vital for sustained recovery and mental wellness.
Preventive Strategies and Public Health Policies
Alongside treatment, public health policies and preventive strategies play a pivotal role in curbing drug-induced mental health issues.
School-based prevention programs that educate youth about the mental health risks of substance abuse have shown positive results in reducing initial experimentation and addiction. Workplace programs that offer mental health support and addiction resources can also help identify issues early.
At the policy level, expanding access to mental healthcare and rehabilitation services through legislation is key to lowering barriers for those at high risk. Policies that curb overprescription of opioids and other addictive substances also help control availability and subsequent abuse.
A multipronged approach across education, workplace settings, and policy is required to strengthen mental health resilience and prevent substance abuse issues.
Case Studies: Recovery and Rehabilitation
Sam Wright struggled with alcohol addiction for over a decade, eventually developing severe depression and attempting suicide. After entering an intensive inpatient rehab program combining group counseling, 12-step meetings, and antidepressants, he has now been sober for 5 years.
For Tanya Singh, a former opioid addict, methadone maintenance treatment along with regular psychiatric visits provide the ongoing support she needs to manage her addiction and bipolar disorder.
These cases demonstrate that with early intervention and sustained treatment, individuals can take control of addiction and any co-occurring mental health disorders. A strong support system improves long-term outcomes.
Emerging Research and Future Directions
As neuroscience continues to uncover new insights into the brain changes linked to addiction and mental illness, researchers are developing innovative treatment approaches.
One area of promise is using transcranial magnetic stimulation (TMS) to normalize irregular brain activity associated with disorders like depression, without surgery or medication (11). TMS may eventually help treat substance abuse as well.
Pharmacogenetic testing to predict individual responses to psychiatric medications based on genetics is also an emerging field that could optimize treatment. Further research on these frontier approaches can pave the way for more targeted and effective treatment.
In the future, a deeper understanding of the biological basis of addiction and mental illness may allow for specialized interventions that help sever their entanglement for good.
FAQs
1. How common is it for individuals with substance abuse disorders to also have mental illness?
The article mentions that nearly 50% of individuals with a substance abuse disorder also suffer from mental illness.
2. How does drug use affect mental health in the short and long term?
The article explores the bidirectional relationship, explaining that mental illnesses like depression and anxiety can precede addiction, while chronic drug use can exacerbate existing mental health conditions or trigger new psychiatric disorders.
3. What are the psychopharmacological effects of stimulants, opioids, and depressants on mental health?
The article details how different drug classes impact mental health, discussing the effects of stimulants, opioids, and depressants on dopamine levels, pain relief, and central nervous system activity.
4. Are the changes in the brain caused by long-term drug use reversible?
The article mentions that some drug-induced brain changes may persist even after quitting the drug due to alterations in brain structure and function.
Conclusion
The interrelationship between substance abuse and mental health is intricate, with each exacerbating vulnerability for the other. A multilayered healthcare approach combining education, prevention, evidence-based treatment, and policy is required to address this public health crisis. While risks persist, recovery is possible with comprehensive long-term treatment, social support, and addressing mental wellness holistically. Emerging solutions offer new hope for the future.
WARNING: The content of this article does not offer any medical advice and is intended for informational purposes only. If you, a friend, or loved one is struggling with substance abuse or mental health issues, please seek professional help immediately. Always consult with your healthcare provider about any health-related decisions. Neither KISS PR nor its distribution partners shall be held responsible for any action taken based on the information provided in this article. Proceed with caution and at your own risk.
Source: Story.KISSPR.com
Release ID: 899130
